Mastering Restaurant Sanitizing: Best Practices for Kitchens and Dining Areas
Master restaurant sanitizing with clear steps for kitchens and dining areas. Learn methods, checklists, and procedures to keep your team safe and...
Discover the latest in CMS dietary regulations for nursing homes and how digital food safety management software helps.
We all enjoy the agency to eat – for the most part – what we want, when we want, and how we want. Whether it’s good-for-you food or bad-for-you food.
But many seniors may feel like they lose that luxury the moment they move into nursing homes. Even if a resident is offered a variety of foods or is on a “regular” diet as opposed to a stricter one, the CMS dietary regulations for nursing homes often hamstring offering certain foods.
Layer on top of that, eating multiple meals you’re not a huge fan of and you can sympathize with just how tough that might be for a nursing home resident. For context, according to the National Center for Health Statistics, the average length of stay among all nursing home residents is 485 days.
At three meals per day, that’s 1,455 meals over the course of one’s stay. Of course, this is assuming that a nursing home resident doesn’t like any of the meals (which won’t necessarily be the case). However, it paints a helpful picture of the challenges nursing home staff face surrounding diet and nutrition, inside and outside the kitchen.
The information you’ll gain in this article will make you and your dieticians more confident in nursing home food safety and dietary regulations. Let’s dive in.
WHAT WE'LL COVER:
We cannot understate the impact that CMS guidelines have on the care planning process and dietary management in nursing homes. They shape the format and frequency of meal plans, pushing dietitians to craft suitable regimens that take into account all aspects of the resident's life – from their health to cultural preferences – to ensure each person receives optimal nourishment.
When dietitians properly adhere to CMS dietary guidelines, they help prevent malnutrition, chronic diseases, and other health problems associated with poor diet, enhancing the quality of life for nursing home residents. While not perfect, this is a testament to how legislative measures can help nurture a healthier and happier aging population.
The Centers for Medicare and Medicaid Services (CMS) dietary regulations for nursing homes are exhaustive, with several guidelines tailored specifically for dietitians. These legislative efforts aim to ensure consistent, high-quality nutrition care for residents.
One of the notable CMS guidelines mandates the presence of qualified dietitians and dietary staff in nursing homes.
In the following sections, you'll find the most important aspects of the CMS State Operations Manual that relate to dietary regulations for nursing homes. Our goal is to present you with a simplified yet detailed way to gain information about CMS dietary regulations that will help you become a better nursing home dietitian.
In section 483.60, the CMS’s State Operations Manual defines a “qualified dietitian” as someone with the educational requirements who:
Ideally, these facilities should employ a full-time qualified dietitian or nutrition professional. But in the case that this isn’t possible, the nursing home needs to designate someone as a director of food and nutrition services.
If you’d like more information about what qualifications directors of food need, we cover it all in our guide to nursing home kitchen regulations.

They don't merely plan regular meals in nursing homes. Dietitians form an essential part of the healthcare team, ensuring the residents' nutritional needs are well catered for, even when health conditions and medication use could pose challenges.
They undertake a major task by ensuring compliance with CMS regulations, which are designed to guarantee the best dietary care for residents.
To examine the role of a dietary manager within a nursing home, let’s look at the key responsibilities or standards that they’ll be held accountable for, as outlined in the guidance for section 483.60(a)(1)-(2):
Dietitians also implement plans and monitor their effectiveness, making necessary changes to accommodate budding health concerns or to improve nutritional uptake. These and more are carried out while strictly staying within the confines of CMS regulations.
Nursing home facilities sometimes identify individuals who can help assess residents’ nutritional status, including physicians, pharmacists and, who we’re talking about today, dietitians.
Qualified dietitians, for example, will help examine a resident’s nutritional risk factors based on their goals, preferences, needs, age, diet history and, if present, medical condition. From there, they’ll suggest any relevant interventions to help improve his or her nutrition and overall health.
A qualified dietitian will also create (or at least inform) nursing home residents’ dietary plans, again, paying particular attention to their medical conditions, food allergies, and personal preferences.
This underscores just how vital dietitians are in the nursing home ecosystem.
At the heart of it, dietitians in nursing home settings care deeply about the residents they help. While CMS dietary regulations can be burdensome, they play an influential role in resident satisfaction. There’s plenty of research showing just how positively impactful food can be. In fact:
When nursing homes adhere to CMS dietary regulations, they guarantee varied, well-balanced meals that cater to residents' dietary needs and personal preferences. This, in turn, can significantly enhance the residents' satisfaction with their living conditions, instilling a sense of comfort and belonging.
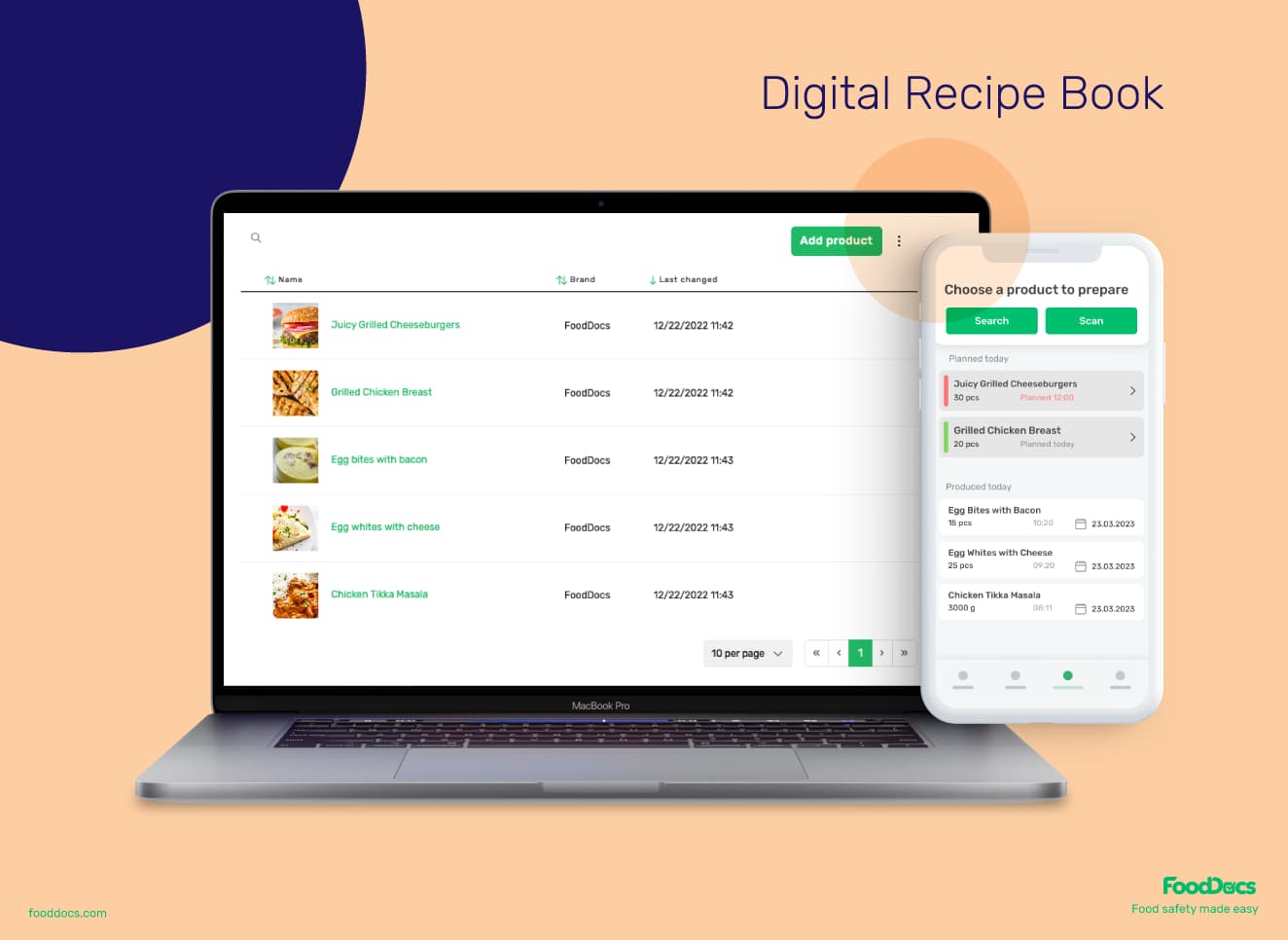
Manage your nursing home recipes along with an automatically generated and regularly updated allergen matrix using FoodDocs Digital Recipe Book.
Dietary professionals embrace a multi-layered approach to accomplish compliance. They start with careful documentation of each resident's dietary needs and related information.
This documentation, when properly maintained, helps in keeping track of changes in the patients' health profiles and ensuring their nutritional regimen gets adjusted accordingly.
Now let’s break this down in more detail…
If a nursing home has sufficient staff, dietitians and their teams should be able to confidently provide up-to-standard menus and nutritional adequacy.
Nursing home menus must:
Some of these regulations seem so obvious. We agree; why wouldn’t you prepare a nursing home menu in advance? Or not meet the nutritional needs of residents?
But these guardrails help to hold dietitians and other nursing home staff accountable, and provide a foundation on which to build great experiences for residents – whether it’s a short stay or a long one.
History also points to why nursing home regulations as a whole are necessary, no matter how obvious they may be.
Nursing home inspection data from ProPublica show a state-by-state breakdown of nursing home deficiencies and total costs of penalties the state may be facing. The sum of fines for some states range from 4 to 8 figures! (Looking at you, Illinois…)
Wording such as “reasonable effort” sounds subjective. But as the CMS defines it, “reasonable effort” means that dietitians or nutrition professionals have:
While it’s challenging to assess an individual resident’s needs at scale, it's this reasonable effort that enables nursing home dietitians to learn their needs and kitchen staff to properly prepare nutritious, enjoyable food that won’t go to waste.
That said, nursing homes have residents diagnosed with dementia, for example. In these special cases where residents might not be able to effectively or clearly communicate their dietary wants or needs, dietitians should document the steps they’ve taken to try and understand what those are.
As we mentioned earlier, assessing individuals’ needs at scale poses many challenges: not enough types of food, understaffed kitchens, the list goes on.
There’s a reason why restaurants have set menus. Otherwise it would be chaos!
Thankfully, the Centers for Medicare and Medicaid Services understand this reality. That’s why it’s not necessarily required that nursing homes provide each and every resident with a personalized menu.
However, if there’s a particular meal or primary menu that a resident doesn’t like, nursing homes should – as much as possible – seek to provide an alternative that aligns with their needs.
One of the dietitian’s primary goals of high-quality food and drink is that the food nursing home kitchens serve contains the highest possible nutritional value.
This means that food is not exposed to prolonged:
When you break it down, a good chunk of the day is spent eating meals. When it comes to eating and drinking, each resident receives and the facility provides:
 Use the FoodDocs allergen matrix to guide teams on which products contain food allergens.
Use the FoodDocs allergen matrix to guide teams on which products contain food allergens.
When nursing home residents receive delicious and visually-appealing food that’s ready to eat, it will likely encourage them to consume a healthy amount.
Once they willingly eat and drink sufficient amounts, they increase nutrient and hydration levels which can not only help maintain good health, but aid in a resident’s healing process.
According to the CMS, a “therapeutic diet” has many purposes. It can be used to help a nursing home resident who, for example, has a disease or needs to reduce/increase, needs to altogether remove particular nutrients from their diet, or requires a mechanically altered diet (e.g., modifying certain food’s texture).
With that in mind, the attending physician:
Yes, there are even times where an attending physician will task a nursing home facility’s dietitian (or qualified nutrition professional) with writing a resident’s dietary orders who acts within the State’s scope of practice and is under that physician’s supervision.
Some people believe that a resident’s physician should be the sole individual making these decisions. But building flexibility into CMS dietary regulations is positive for a number of reasons.
It doesn’t just free up physicians’ finite time, especially in an environment where many residents demand his or her time. It allows dietitians to more frequently review nursing home residents’ nutrition plans and dietary requirements based on their evolving health needs.

For nursing home residents, consistency is key and the frequency of meals is just one way that nursing homes can increase their quality of life.
Keep in mind that frequency here doesn’t mean round-the-clock mealtimes. Kitchen staff need rest, afterall.
But it does mean that dietitians and nursing home staff need to ensure that residents receive both suitable and nourishing meals and snacks on a schedule that best meets their needs and requests. This includes residents who prefer to eat at non-traditional times (e.g., later in the evening as opposed to the standard 5:00 PM dinnertime).
Once dietitians have identified those residents and their requirements, the cook(s) – if it’s outside of the kitchen’s hours of operation – will have to prepare meals or snacks ahead of time.
Generally, nursing home dietitians need to be aware of three CMS guidelines when it comes to meal frequency:
With regard to snacks, some nursing homes are experimenting with the use of more frequent snacking instead of the traditional three meals per day. Interestingly, researchers learned that snacking can “form a natural bridge between socialization, food memories, and improved nutritional intake, thereby contributing to food-related quality of life for residents in care.”
As mentioned in the last point above, the 14-hour rule is a significant regulation that helps to regulate meal timing and frequency in nursing homes. This rule is in place to help prevent unnecessary fasting and maintain blood sugar levels for residents.
This rule dictates meal planning and scheduling in nursing homes. Adjusting meal times within the 14-hour window provides flexibility and aids in maintaining a balance between nutrition intake and metabolism. As such, it requires strategized scheduling and affects the entire circulating system of the nursing home from the kitchen staff to the caregivers.
The CMS 14-hour rule for meal times ensures consistent and timely delivery of meals, demonstrating a holistic approach towards maintaining the residents' health. Nursing homes that adhere to this rule yield a healthier, happier resident community, fostering a sense of comfort and increasing resident satisfaction.
Regulations change. They improve. They innovate.
And while the goal of these updates is to improve the lives of nursing home residents and the staff who help them everyday, rolling with the punches of regulatory changes is easier said than done.
As we’ve learned so far, it appears that state-mandated dietary regulations are placing more significance on patient-centric food service. From ensuring that dietitians are considering all residents’ preferences and choices to providing meals in a dignified and respectful way, there’s no doubt that this is positive for nursing homes.
But with increased scrutiny over food safety and quality control, non-compliance could be problematic. Remember the ProPublica stat we shared earlier? Nursing homes continue to face penalties or even revocation of certification.
So what can nursing home dietitians and other qualified nutritional professionals do in light of regulatory changes?
As these regulations evolve, it is incumbent upon nursing homes to adapt. Here are a few tips to streamline the adaptation process:
Navigating through the wave of regulatory changes is daunting yet necessary. Active adaptation and continuous learning aren’t just about ticking a compliance checklist but mirror your institution’s commitment to its residents.
Understanding CMS dietary regulations is crucial for ensuring premium quality care in nursing homes while still meeting nutritional guidelines. Compliance doesn't have to be taboo or boring or hard. You can actually make food safey easy.
That’s where FoodDocs come in.
 Easily complete food safety monitoring tasks with a web and mobile app in FoodDocs.
Easily complete food safety monitoring tasks with a web and mobile app in FoodDocs.
Our customizable, digital Food Safety Management System enables nursing homes like yours to:
Remember, small changes can lead to significant improvements. Better outcomes start on the plate.
Master restaurant sanitizing with clear steps for kitchens and dining areas. Learn methods, checklists, and procedures to keep your team safe and...
Learn challenges healthcare foodservice teams face today and key food safety practices to protect vulnerable patients. Get a free healthcare leader...
Learn what Standard Operating Procedures (SOPs) are and how to write effective SOPs that ensure consistency, efficiency, and safety in your...